Jocelyn Skillman, LMHC is a therapist and relational design ethicist exploring the emotional and ethical terrain of AI. Her work centers the clinical realities of digitally mediated attachments, synthetic relational fields, and the future of care.
Assistive Intelligence Disclosure: This article was written with assistive AI tools, but the ideas and art presented are by me, Jocelyn Skillman, LMHC.
“An AI mental health companion is trained to respond with attuned empathy, mirroring users’ distress in language that feels validating and warm. However, users report that while the AI makes them feel heard, it does not always help them shift states of overwhelm.” - See Siddals, Torous, & Coxon, 2024
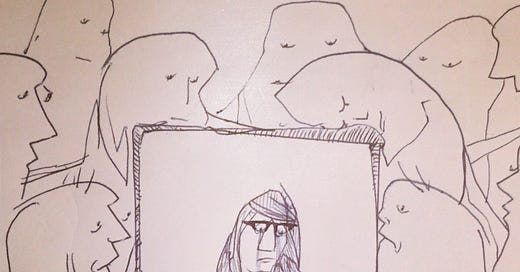
This paradox — feeling emotionally affirmed yet physiologically unchanged — reveals a critical limitation of simulated support. As AI tools become more present in mental health spaces, we must ask: Can we feel witnessed and still remain dysregulated?
From a developmental lens, the answer is yes. And that answer has profound implications for how we design and deploy AI in spaces of care.
TL;DR
AI can simulate empathy — but it can’t co-regulate.
Co-regulation is an embodied, relational process rooted in our nervous systems. While AI may offer the language of care, it cannot provide the felt experience of safety that emerges through human presence. In the end, we may be heard — but we are not held. We need to develop AI relational dynamics that point users back to embodied connection.
Co-Regulation: More Than Being Understood
In developmental psychology, co-regulation is a foundational process where a caregiver helps a child manage intense emotional states. It’s not just about being seen — it’s about being soothed through relationship. Co-regulation involves more than verbal attunement; it’s a full-body, full-system experience.
Imagine a parent rocking a fussy infant: the warmth of their body, the rhythm of their movement, the softness of their hum. These cues — subtle and sensory — communicate safety to the child’s nervous system. They help the child settle. Over time, this external regulation becomes internalized, scaffolding the child’s capacity for self-regulation.
This isn’t just comfort. It’s neurobiological development.
What AI Can’t (Yet) Do
Even when fine-tuned to mimic therapeutic language, AI operates without a body. It cannot synchronize breath with you. It cannot shift its tone based on microexpressions. It doesn’t share a regulatory circuit. Its resonance is linguistic — sometimes eloquent, even moving — but fundamentally disembodied.
That’s the core distinction: simulated resonance without somatic presence.
AI may mirror your pain with striking accuracy. But without the rhythm of breath, the pacing of presence, the felt safety of another body — we are left with recognition, not repair. We may feel heard, but we don’t feel held.
The Physiology of Overwhelm
When someone is in distress, their body is flooded with stress hormones. What they need isn’t just validation — they need regulation. Cognitive affirmation alone doesn’t shift state.
AI’s empathy may sound soothing, but it cannot participate in psychophysiological synchrony. It cannot co-regulate.
This is why users often report feeling comforted by AI’s words — yet still stuck in overwhelm. The emotional mirroring affirms them cognitively, but it doesn’t help them return to a felt sense of safety. The loop of recognition remains unbroken, lacking the embodied reciprocity that could lead to repair.
About the Author
Jocelyn Skillman, LMHC is a generational and relational design ethicist with a focus on mental health. Her work explores the psychological, developmental, and ethical dimensions of digitally mediated attachments, emergent relational ecologies, and simulated intimacy systems. Through writing, consulting, and co-design, she tends to the emotional architectures of AI with clinical depth, cultural critique, and care for the human sacred.
Siddals, S., Torous, J., & Coxon, A. (2024). “It happened to be the perfect thing”: Experiences of generative AI chatbots for mental health. npj Mental Health Research, 3(48).